A nephrectomy surgery — the removal of a kidney — is usually needed only in serious or unavoidable medical conditions.
1. Kidney Cancer
2. Severely Damaged Kidney
3. Chronic Kidney Infection
4. Uncontrolled High Blood Pressure (Renovascular Hypertension)
5. Congenital Kidney Abnormalities
6. Living Kidney Donation
7. Severe Trauma
Nephrectomy Surgery – Step-by-Step Procedure
1. Preoperative Preparation
Patient is admitted and evaluated.
Imaging (CT scan, MRI) confirms the need for kidney removal.
Anesthesia team reviews and prepares the patient.
Patient fasts for 6–8 hours before surgery.
2. General Anesthesia
Patient is put to sleep completely.
A breathing tube is placed to support breathing during surgery.
3. Patient Positioning
The patient is usually placed in a side-lying position (flank position), depending on which kidney is being removed.
The area is sterilized and draped for surgery.
4. Surgical Incision
There are two types of approaches:
a) Laparoscopic Nephrectomy (Minimally Invasive)
3 to 4 small cuts are made.
A camera and surgical instruments are inserted through the cuts.
Gas (CO₂) inflates the abdomen to improve visibility.
b) Open Nephrectomy
A larger cut (10–20 cm) is made on the side or abdomen, or back.
Used for large tumors, complex cases, or trauma.
5. Dissection and Removal
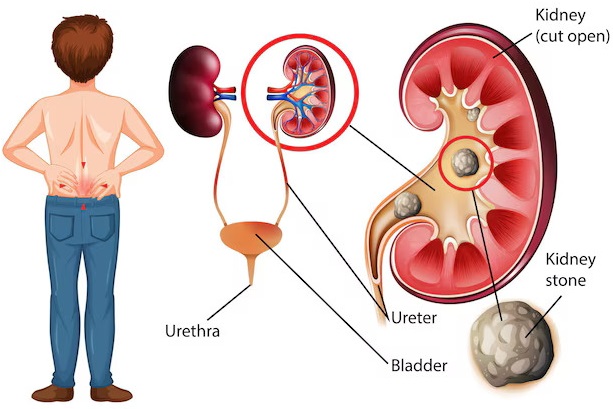
The surgeon carefully separates the kidney from:
Fat and surrounding tissues
Renal artery and vein (blood vessels)
Ureter (urine tube)
Blood vessels and ureter are clamped, cut, and sealed.
6. Kidney Removal
In radical nephrectomy: the entire kidney (plus adrenal gland and surrounding fat, if needed) is removed.
In partial nephrectomy: only the diseased part of the kidney is removed.
In laparoscopic cases, the kidney is placed in a specimen retrieval bag and removed through one incision.
7. Closure
Bleeding is checked and controlled.
A drain tube may be placed.
All incisions are closed with stitches or surgical staples.
A sterile dressing is applied.
8. Recovery
Patient is monitored in recovery room.
Pain medications and IV fluids given.
Urinary catheter usually placed temporarily.
Gradual return to eating, walking, and normal activities.
Discharge in 2–5 days (laparoscopic) or up to 7 days (open surgery).