Bladder Augmentation is needed when the bladder is too small, stiff, or unable to store urine properly, causing serious problems.
Bladder Augmentation is needed when:
Bladder cannot hold enough urine (small bladder capacity).
Bladder is too stiff or high-pressure, risking kidney damage.
Severe urinary incontinence that doesn’t improve with medication or catheter use.
Neurogenic bladder (due to spinal cord injury, spina bifida, etc.).
Congenital bladder problems like bladder exstrophy or other birth defects.
Chronic bladder inflammation or damage from radiation, infection, or long-term catheter use.
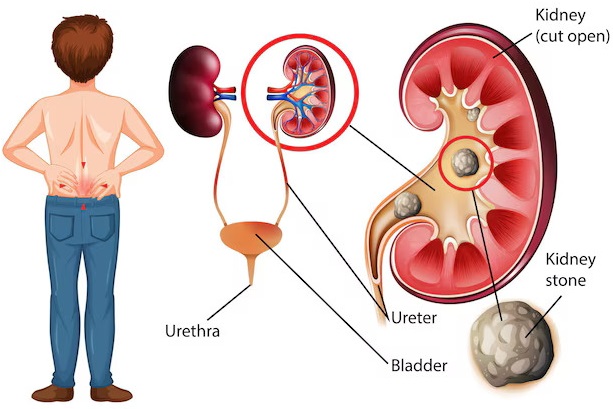
Urine backing up to kidneys (vesicoureteral reflux) due to poor bladder function.
Procedure of Bladder Augmentation (Augmentation Cystoplasty)
1. Anesthesia
The patient is placed under general anesthesia (completely unconscious).
2. Opening the Abdomen
A surgical incision is made in the lower abdomen to access the bladder.
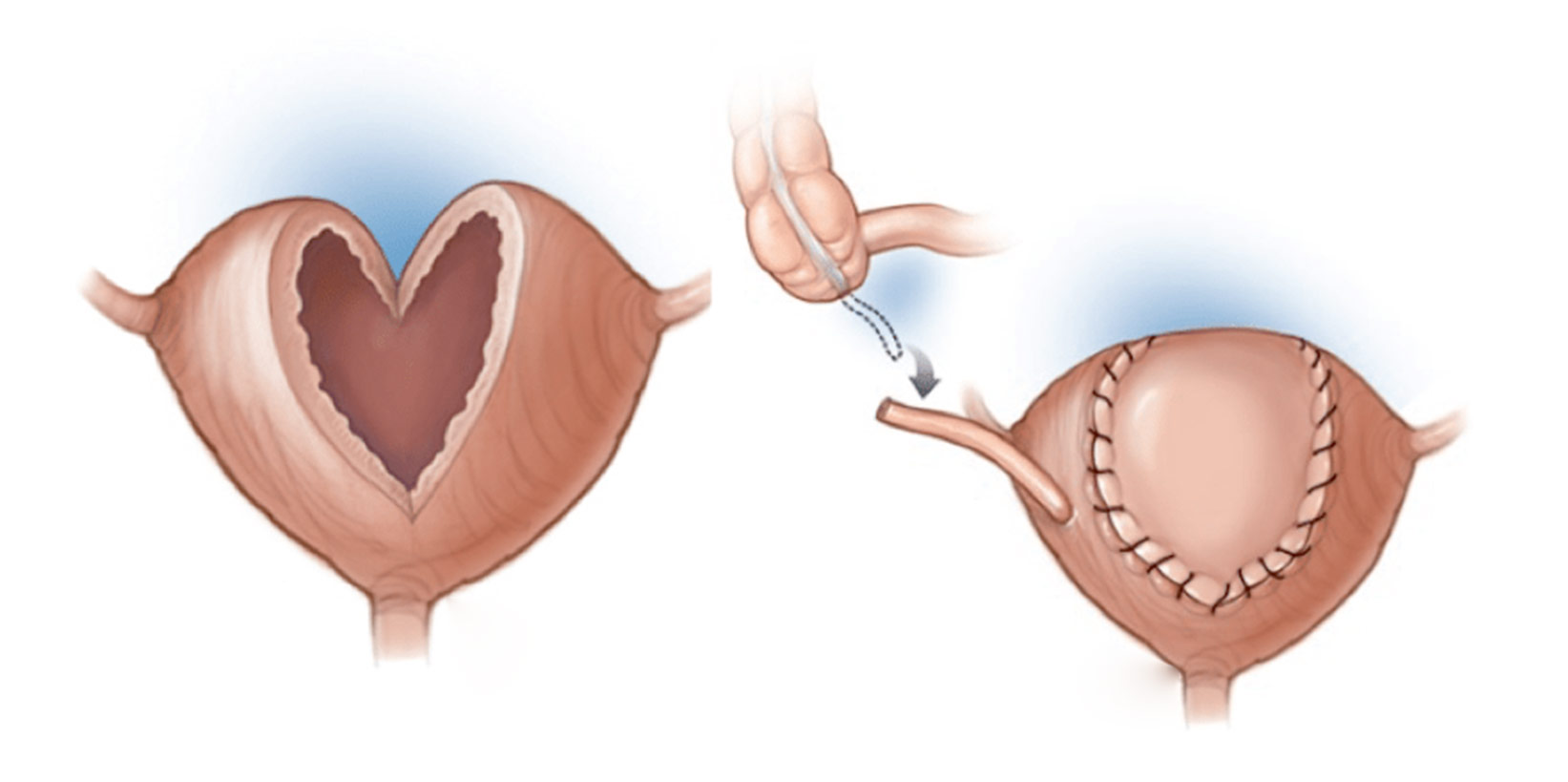
3. Opening the Bladder
The surgeon cuts open the bladder at the top to prepare it for expansion.
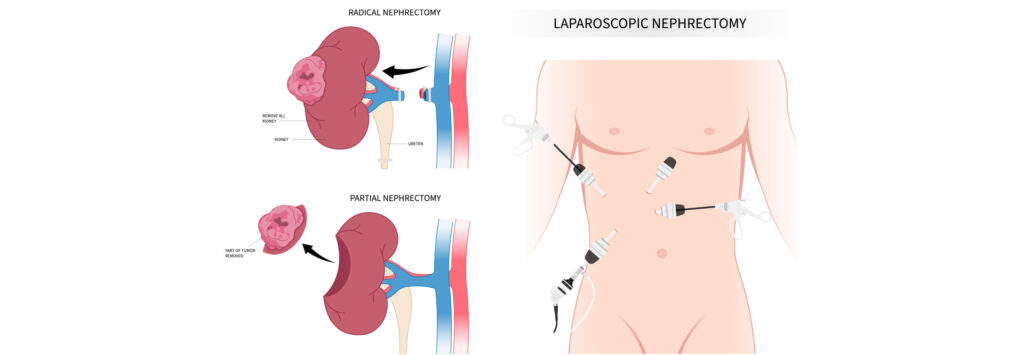
4. Removing a Section of Intestine
A small piece of intestine (usually ileum) is removed.
The intestine is then reconnected so digestion continues normally.
5. Attaching Intestine to Bladder
The intestinal segment is reshaped and sewn to the bladder to increase its size and reduce pressure.
6. Closing the Incision
A catheter is placed into the bladder to drain urine.
The abdominal incision is closed with stitches.
7. Post-Surgery Recovery
Hospital stay: 7–10 days.
Catheter use: 2–3 weeks.
Patient may need to learn self-catheterization for bladder emptying.
Benefits
Increased bladder capacity – can hold more urine comfortably.
Reduced bladder pressure – protects the kidneys from damage.
Improved continence – helps control urine leakage.
Better quality of life – less urgency, fewer infections, and more independence.