Glaucoma is a group of eye diseases that damage the optic nerve, often due to increased intraocular pressure (IOP). Left untreated, glaucoma can lead to permanent vision loss and even blindness. While medications and laser treatments are common first-line therapies, surgery may be necessary when these options are not sufficient.
Who Needs Glaucoma Surgery?
Glaucoma surgery is typically recommended for patients who:
- Have progressive optic nerve damage despite medication.
- Cannot tolerate glaucoma medications due to side effects.
- Have very high intraocular pressure that poses an immediate risk to vision.
What Happens During Glaucoma Surgery?
The exact steps depend on the type of glaucoma surgery being performed, but the main goal is the same: reduce intraocular pressure (IOP) to protect the optic nerve.
- Preparation
- The patient is usually given local anesthesia to numb the eye.
- In some cases, mild sedation may be used to help the patient relax.
- The eye is cleaned and draped in a sterile manner.
- Surgical Procedure
- a) Trabeculectomy
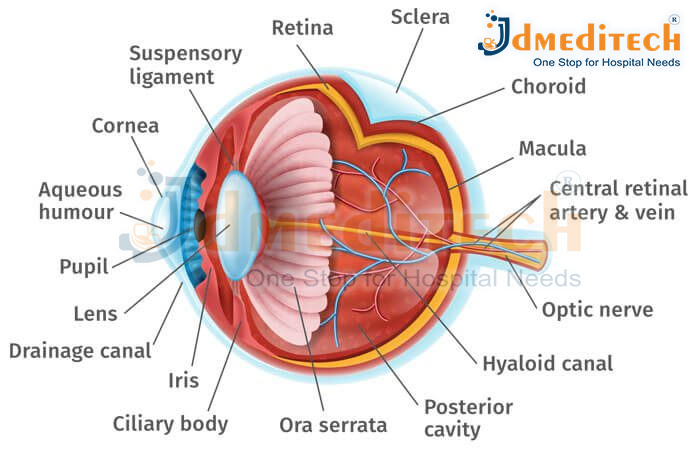
- A small flap is created in the white part of the eye (sclera).
- A tiny opening is made under the flap to allow fluid (aqueous humor) to drain from inside the eye to a small reservoir under the conjunctiva (the thin membrane covering the eye).
- This helps lower eye pressure.
- b) Glaucoma Drainage Device (Tube or Shunt)
- A tiny tube or implant is placed to direct excess fluid out of the eye.
- The device is positioned so that fluid drains safely, reducing pressure.
- c) Minimally Invasive Glaucoma Surgery (MIGS)
- Small stents or micro-devices are inserted into the eye’s drainage channels.
- These procedures are less invasive and usually combined with cataract surgery.
- d) Laser Surgery
- A laser is used to improve fluid drainage:
- Trabeculoplasty: Opens the drainage meshwork.
- Iridotomy: Creates a tiny hole in the iris to relieve pressure in angle-closure glaucoma.
- Closing and Recovery
- In traditional surgeries, the flap or incision is carefully closed.
- Antibiotic or anti-inflammatory eye drops are applied.
- A protective eye patch or shield may be used temporarily.
- After Surgery
- Most patients go home the same day.
- Eye drops are prescribed to prevent infection and control inflammation.
- Follow-up visits are critical to monitor eye pressure and healing.
Types of Glaucoma Surgery
There are several surgical options available depending on the type and severity of glaucoma:
Trabeculectomy
- Creates a small drainage flap to allow fluid to escape from the eye, reducing intraocular pressure.
- One of the most common glaucoma surgeries with proven long-term effectiveness.
Glaucoma Drainage Implants (Shunts or Tubes)
- Devices implanted to help drain excess eye fluid.
- Usually considered for patients who have failed other treatments or have complex glaucoma.
Minimally Invasive Glaucoma Surgery (MIGS)
- Newer procedures that are less invasive and have faster recovery times.
- Often combined with cataract surgery.
- Examples include iStent, Xen Gel Stent, and Hydrus microstent.
Laser Surgeries
- Laser Trabeculoplasty: Helps improve drainage through the eye’s natural drainage system.
- Laser Iridotomy: Primarily for angle-closure glaucoma, creating a small hole in the iris to improve fluid flow.
Before
Before undergoing surgery, the medical staff will prepare you mentally to ensure you’re comfortable. You will then go to the operation room, where you will lie on the operating table.
In the room, there will be an eye surgeon, a nurse, and surgical assistants.
Your eyes will be cleaned and your face covered, leaving only the infected eye exposed.
Your doctor will also install devices to monitor your heart rate, blood pressure, and oxygen levels throughout the procedure.
An anesthesiologist will also be present to administer sedatives to keep you relaxed during surgery.
After
After surgery, you’ll be allowed to rest your eyes for a moment.
During this time, your eye doctor will continuously monitor your eye pressure. If everything seems okay, you’ll be discharged.
However, before you leave, the eye doctor will instruct you on the dos and don’ts after glaucoma surgery.
You may also be required to schedule a follow-up appointment.
After glaucoma surgery, your eye will be patched up for some time. This may affect your ability to see. In addition, the effects of sedation also affect your ability to operate machinery.