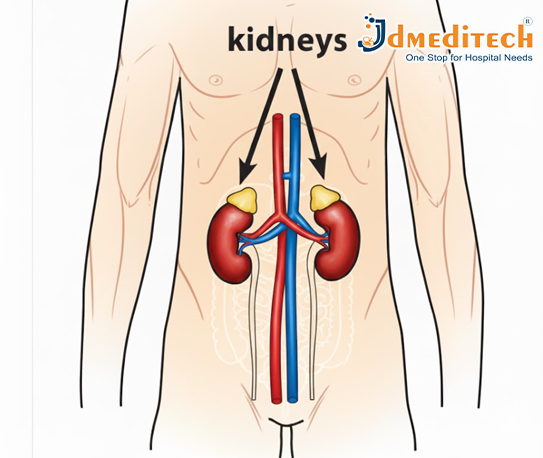
What Is Chronic Kidney Disease?
Chronic Kidney Disease (CKD) is a long-term health condition in which the kidneys slowly lose their ability to function properly over time. The kidneys are responsible for filtering waste products, toxins, and excess fluid from the blood. When they become damaged, these harmful substances start to build up in the body, leading to serious health problems.
CKD develops gradually, often over months or years, and may not show noticeable symptoms in its early stages. As the disease progresses, kidney function continues to decline, eventually leading to End-Stage Renal Disease (ESRD)—a stage where the kidneys can no longer support the body’s needs. At this point, patients require dialysis or a kidney transplant to survive.
What are the symptoms of CKD?
Chronic Kidney Disease (CKD) is a progressive condition, and its symptoms often appear gradually as kidney function deteriorates. In the early stages, CKD may not show any noticeable symptoms because the kidneys can still compensate for minor damage. However, as the disease progresses, the buildup of toxins, excess fluid, and electrolyte imbalance leads to a variety of physical and metabolic symptoms.
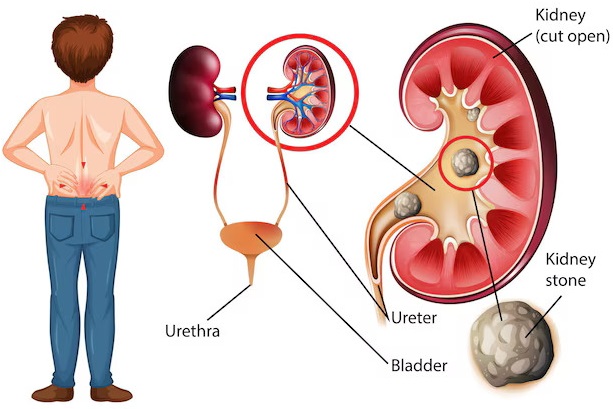
Patients may begin experiencing persistent fatigue, weakness, and lack of energy due to anemia and toxin accumulation. Swelling in the feet, ankles, hands, and face is common as the kidneys lose their ability to remove extra fluid. Many individuals notice changes in urination, such as foamy urine, increased nighttime urination, or reduced urine output.
Other symptoms include nausea, vomiting, loss of appetite, and a metallic taste, which result from rising waste levels in the bloodstream. High blood pressure, muscle cramps, itchy or dry skin, and difficulty concentrating also indicate declining kidney function. In advanced stages, CKD can lead to breathlessness, severe fluid retention, chest discomfort, and almost no urine production, signaling the onset of kidney failure.
Recognizing these symptoms early and seeking medical evaluation can significantly slow disease progression and improve long-term outcomes.
Symptoms of advanced CKD
Common Symptoms of Advanced CKD (Stage 4–5)
1. Severe Fatigue and Weakness
Due to anemia and toxin buildup, patients feel extremely tired and weak and lack energy.
2. Swelling (Edema)
Significant swelling appears in the legs, ankles, feet, hands, and sometimes around the face due to fluid retention.
3. Very Little or No Urine Output
The kidneys fail to produce normal amounts of urine, even though fluid is building up inside the body.
4. Shortness of Breath
Fluid buildup in the lungs causes difficulty breathing, even while resting.
5. Nausea and Frequent Vomiting
Excess waste in the bloodstream leads to digestive discomfort, nausea, and loss of appetite.
6. Extreme Itching (Uremic Pruritus)
High levels of waste products cause persistent and sometimes severe itching.
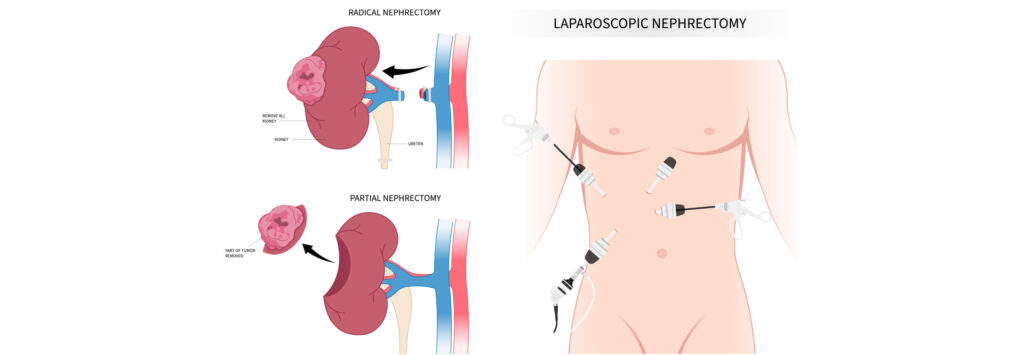
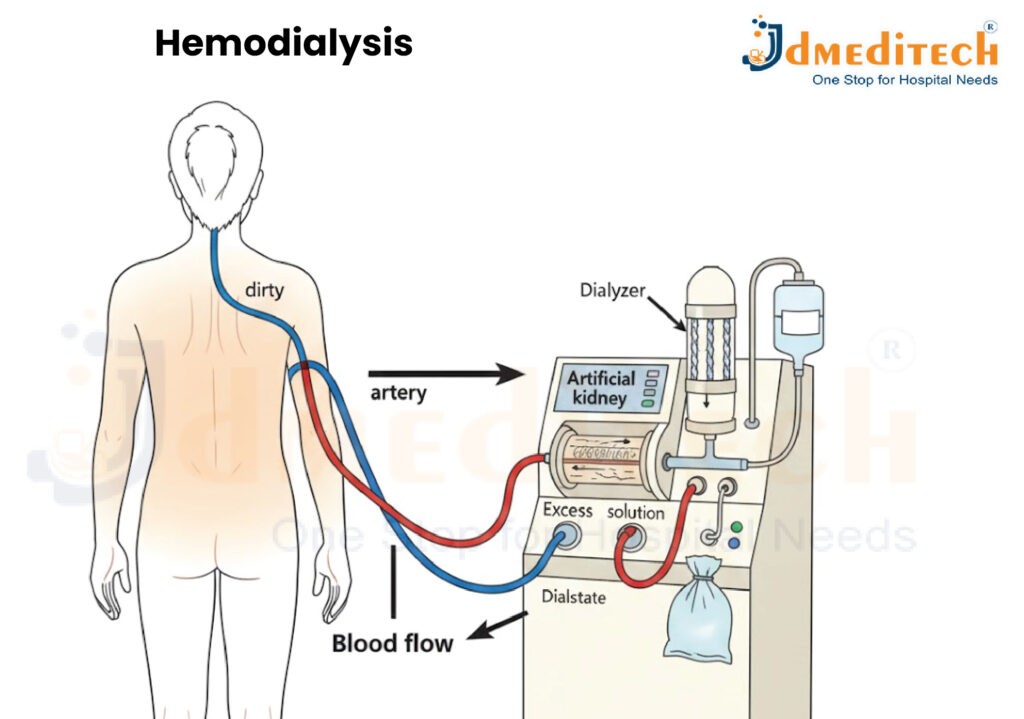
What Is Hemodialysis?
Hemodialysis is a medical procedure used to remove waste products, toxins, and excess fluid from the blood when the kidneys are no longer able to perform these functions effectively. It acts as an artificial kidney for people with advanced Chronic Kidney Disease (CKD) or kidney failure.
During hemodialysis, blood is taken out of the body, cleaned using a machine called a dialyzer, and then returned to the body. This process helps maintain fluid balance, remove harmful substances, and keep electrolytes like potassium and sodium at healthy levels.
How Does Hemodialysis Work?
1. A vascular access (fistula, graft, or catheter) is created to allow blood to flow in and out of the body.
2. Blood travels through tubing into the dialysis machine.
3. Inside the dialyzer, the blood passes through a special filter that removes waste and excess water.
4. Clean blood is then returned to the body through the same access.
5. This cycle continues for the duration of the session.
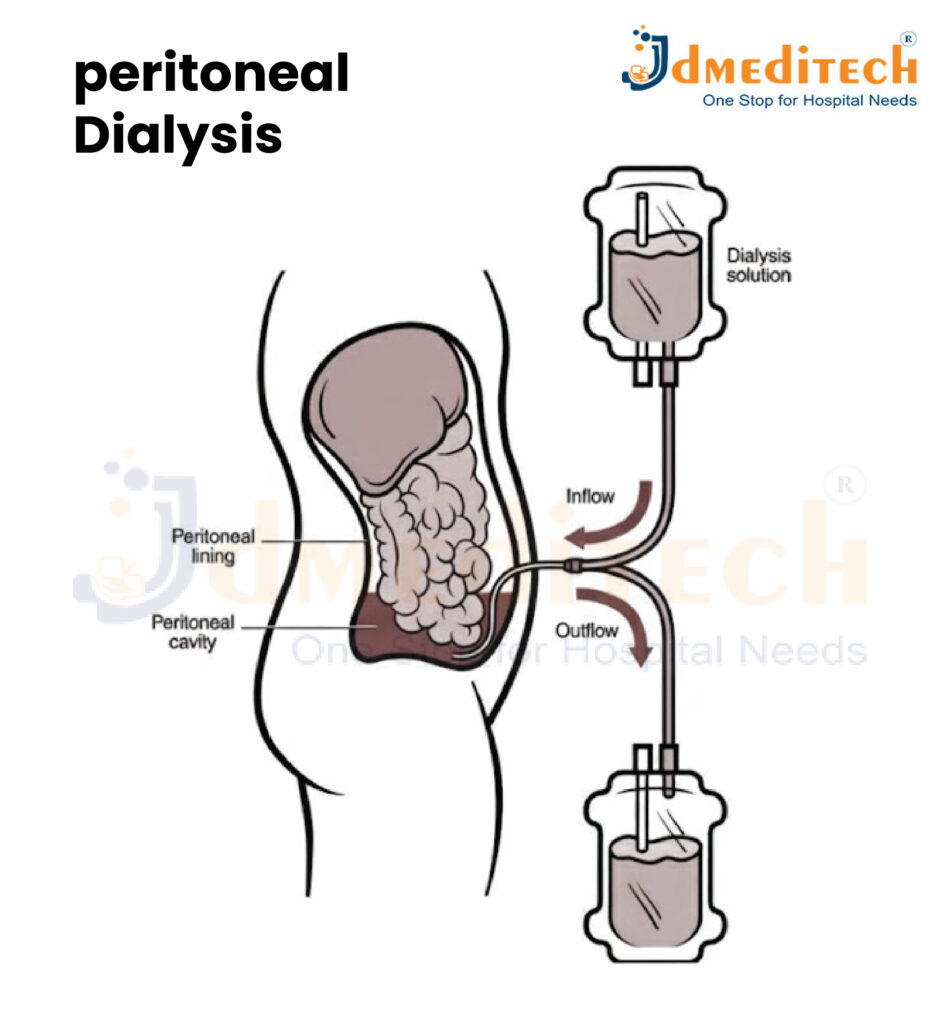
What Is Peritoneal Dialysis?
Peritoneal dialysis (PD) is a type of dialysis that uses the lining of your abdomen—called the peritoneal membrane—to filter waste and excess fluid from the blood. Instead of using a machine like hemodialysis, this method relies on the body’s natural membrane as a filter.
A sterile dialysis fluid is introduced into the abdominal cavity through a soft tube called a peritoneal dialysis catheter. Waste products pass from the blood into the fluid. After a few hours, the used fluid is drained out and replaced with fresh solution.
Peritoneal dialysis is often done at home, giving patients more flexibility and independence.
Types of Peritoneal Dialysis
1. Continuous Ambulatory Peritoneal Dialysis (CAPD)
• Manual process
• No machine required
• Usually 3–4 exchanges per day
• The patient can walk and do daily activities while fluid is inside the abdomen
2. Automated Peritoneal Dialysis (APD)
• Performed using a machine called a cycler
• Usually done at night while the patient sleeps
• More convenient for many people
What Happens During Peritoneal Dialysis?
Peritoneal dialysis (PD) cleans the blood by using the natural lining of the abdomen—the peritoneal membrane—as a filter. The process happens inside the body and does not require blood to leave the bloodstream. Instead, a special cleansing fluid removes waste and extra fluid.
Conclusion
Chronic kidney disease is a progressive condition that requires timely diagnosis and continuous management. When the kidneys fail, dialysis becomes essential to sustain life. Understanding different types of dialysis and how they work helps patients and families make informed healthcare decisions.
With proper treatment, lifestyle changes, and regular follow-up, CKD patients can lead stable and meaningful lives while preparing for the possibility of a kidney transplant.
Hemodialysis SETUP