Breast cancer is one of the most common cancers affecting women worldwide. It develops when abnormal cells in the breast begin to grow uncontrollably, forming a tumor. While breast cancer mainly affects women, men can also develop it, though less commonly. Early detection and timely treatment significantly improve the chances of recovery.
What Is Breast Cancer?
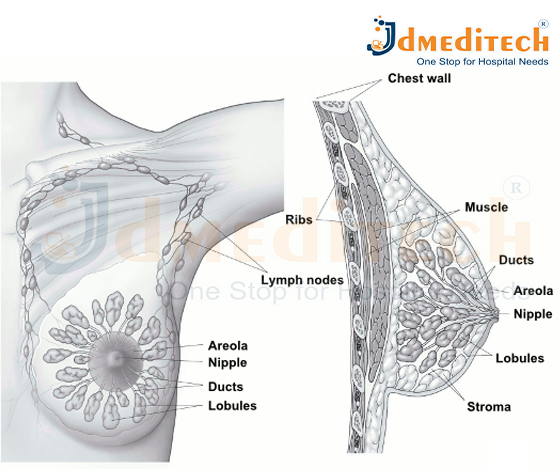
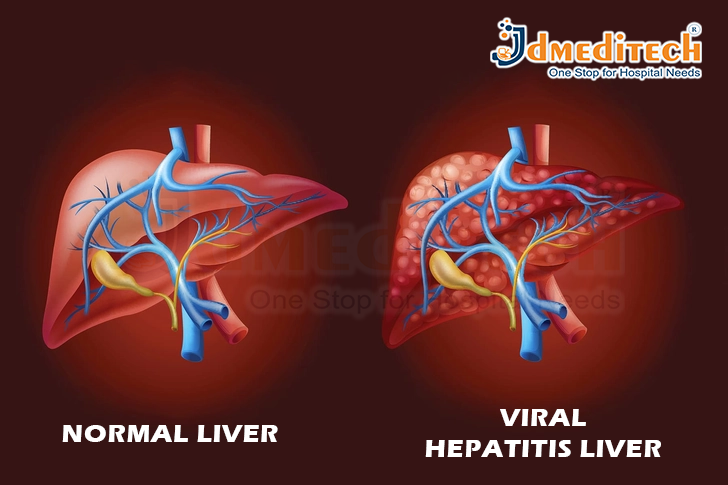
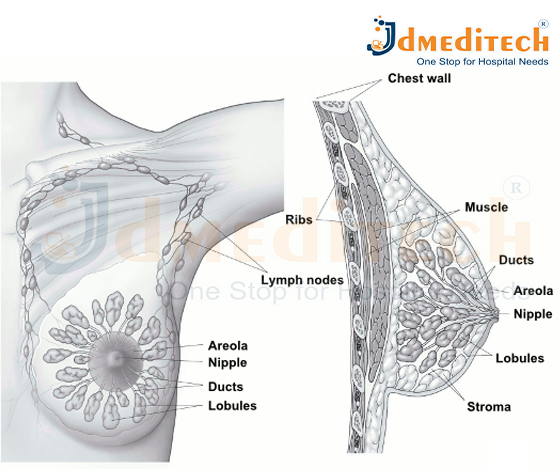
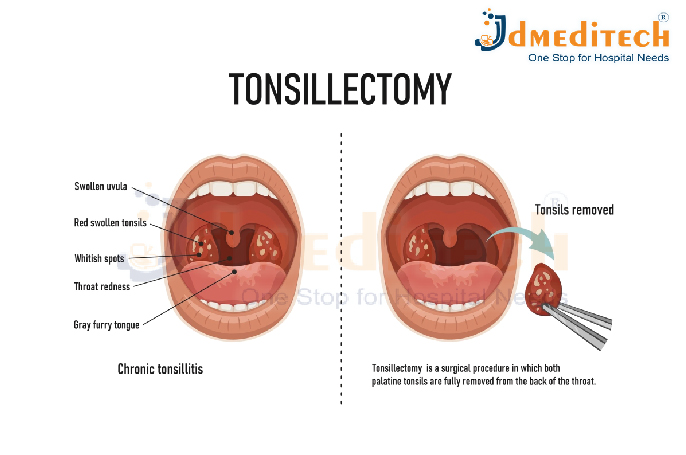
Breast cancer begins in the breast tissue, usually in the milk ducts (ductal cancer) or the milk-producing glands (lobular cancer). These abnormal cells can invade nearby tissues and, in advanced stages, spread to other parts of the body (metastasis).
Breast cancer can vary from slow-growing forms to aggressive types that spread quickly. Understanding your risk and recognizing early signs can help with early diagnosis and better treatment outcomes.
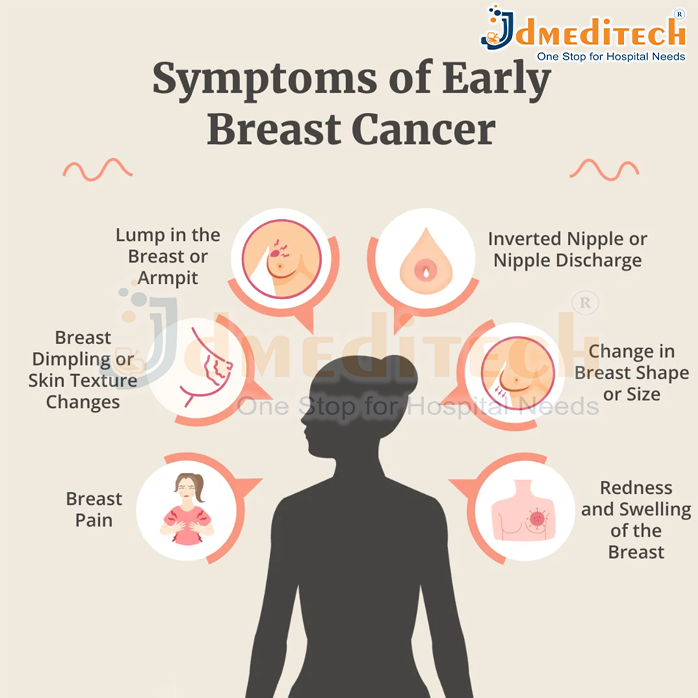
Symptoms of Breast Cancer
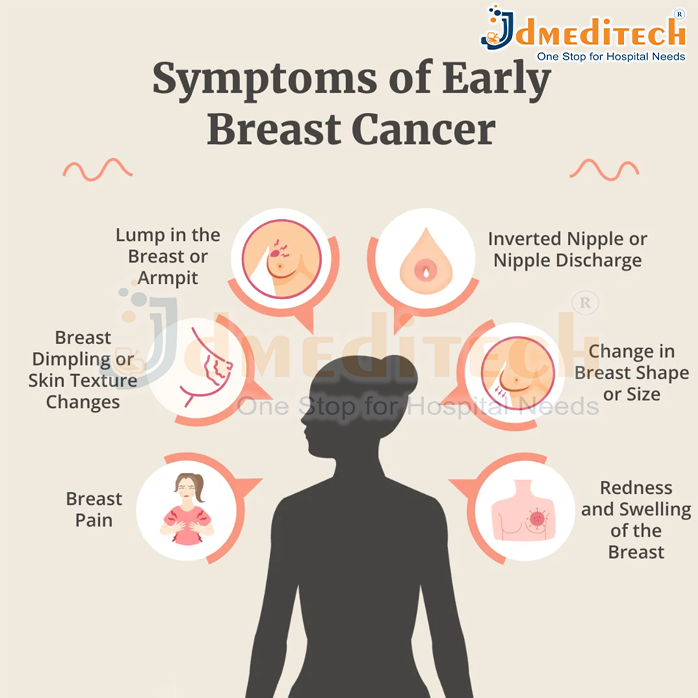
Breast cancer may not cause symptoms in its early stages. However, common signs include:
- A lump or thickening in the breast or underarm
- Changes in the size or shape of the breast
- Nipple discharge (especially bloody)
- Pain in any part of the breast
- Skin changes such as redness, dimpling, or puckering
- Inverted nipple or changes around the nipple area
How Does Breast Cancer Spread?
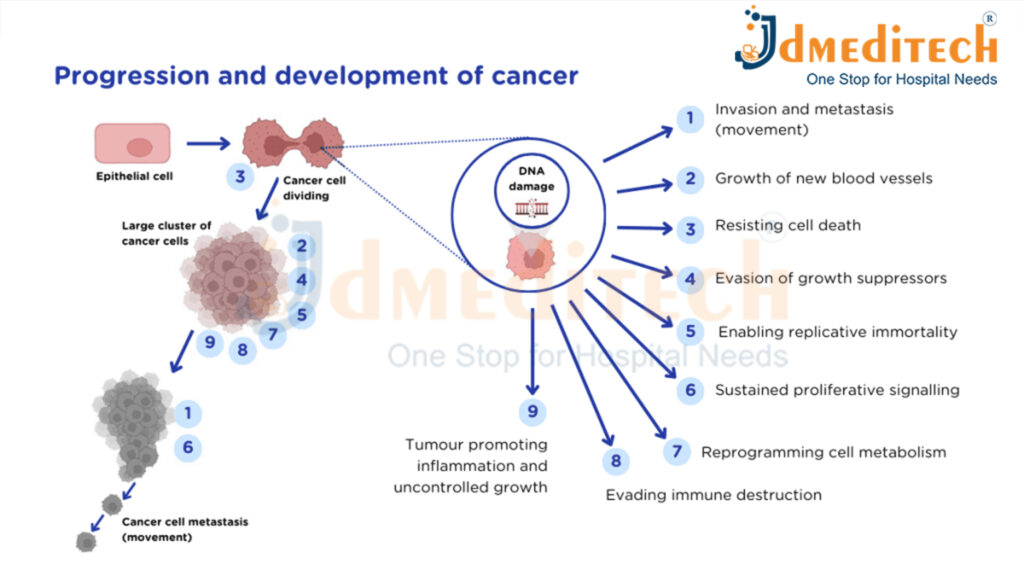
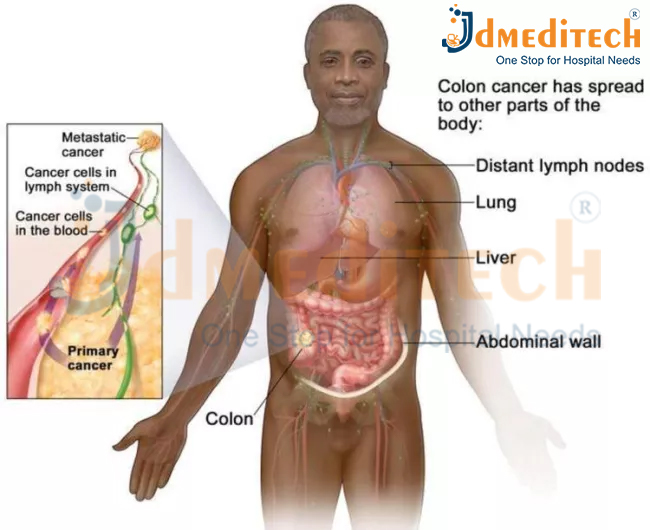
Breast cancer spreads when abnormal cells in the breast grow uncontrollably and begin to move beyond their original location. This process is known as metastasis. Cancer cells can break away from the primary tumor, travel through the body, and form new tumors in other organs. Breast cancer mainly spreads through the following pathways:
-
Lymphatic System
The most common route of spread.
Cancer cells enter nearby lymph nodes—usually in the armpit (axillary nodes), collarbone, or chest—and from there, they travel to other parts of the body.
-
Bloodstream
Cancer cells can also enter the blood vessels and circulate throughout the body. Through the bloodstream, breast cancer can reach major organs such as the lungs, liver, bones, and brain.
-
Direct Spread to Nearby Tissues
As the tumor grows, it can invade nearby structures such as the skin, chest wall, or muscles around the breast.
When breast cancer spreads to distant organs, it is called metastatic or stage 4 breast cancer, even if the new tumors are found in other parts of the body. Early detection and treatment help stop or slow down the spread, improving survival and quality of life.
Types of breast cancer
- Ductal Carcinoma In Situ (DCIS)
A non-invasive cancer where abnormal cells are found in the lining of the milk ducts but haven’t spread outside the duct.
DCIS is considered an early form of breast cancer and is highly treatable.
-
Invasive Ductal Carcinoma (IDC)
The most common type of breast cancer.
IDC begins in the milk ducts and then invades surrounding breast tissue. It may spread to lymph nodes or other parts of the body if untreated.
-
Invasive Lobular Carcinoma (ILC)
Starts in the milk-producing glands (lobules) and spreads to nearby tissues.
ILC can be harder to detect on imaging because of its growth pattern.
-
Lobular Carcinoma In Situ (LCIS)
LCIS is not considered true cancer but a marker of increased breast cancer risk.
Abnormal cells stay within the lobules without invading nearby tissues.
-
Triple-Negative Breast Cancer (TNBC)
A fast-growing type that does not have estrogen, progesterone, or HER2 receptors.
TNBC is aggressive and often requires chemotherapy because hormone therapies do not work on it.
-
HER2-Positive Breast Cancer
This type has high levels of the HER2 protein, causing rapid cancer cell growth.
Targeted therapies (like trastuzumab) are very effective for HER2-positive cancers.
-
Inflammatory Breast Cancer (IBC)
A rare and aggressive form where cancer cells block lymph vessels in the breast skin.
It causes redness, swelling, and a warm feeling—often without a lump.
-
Paget’s Disease of the Breast
A rare cancer that affects the nipple and areola.
It often appears as flaky, red, or irritated skin and is usually linked to underlying DCIS or IDC.
-
Metastatic Breast Cancer (Stage 4)
Occurs when cancer spreads to other organs like the bones, liver, lungs, or brain.
It is not a different disease but an advanced stage of breast cancer.
-
Recurrent Breast Cancer
Cancer that returns months or years after treatment.
It can come back in the breast (loc
al), nearby lymph nodes (regional), or distant organs (distant recurrence).
What Causes Breast Cancer?
The exact cause of breast cancer is not fully known. Breast cancer develops when cells in the breast begin to grow abnormally. These cells divide faster than healthy cells and can form a lump or mass. Over time, they may spread to nearby tissues or other parts of the body. While the specific trigger for this abnormal growth is still unclear, several factors can increase the likelihood of developing breast cancer.
-
Genetic Changes
Certain inherited gene mutations—especially BRCA1 and BRCA2—significantly increase the risk of breast and ovarian cancer. A family history of breast cancer also suggests a higher chance of developing the disease.
-
Hormonal Influence
Estrogen and progesterone levels in the body play a major role. Conditions or treatments that increase exposure to these hormones—such as early periods, late menopause, or hormone replacement therapy—can raise the risk.
-
Age and Gender
Breast cancer is more common in women, and the risk increases with age, especially after 40.
-
Lifestyle Factors
Certain habits or health conditions can contribute to breast cancer risk:
- Obesity
- Lack of physical activity
- Smoking
- Excessive alcohol consumption
- High-fat or processed diet
-
Radiation Exposure
Previous radiation therapy to the chest area—especially during childhood or teenage years—can increase breast cancer risk later in life.
-
Reproductive Factors
- Having the first child after age 30
- Not breastfeeding
- Never having a full-term pregnancy
These can slightly increase the risk due to longer exposure to hormones.
-
Dense Breast Tissue
Women with dense breasts have more glandular tissue than fatty tissue, which can make tumors harder to spot and slightly increase risk.
How Is Breast Cancer Diagnosed?
Diagnosing breast cancer involves a combination of physical examination, imaging tests, and tissue analysis. Early diagnosis is crucial because it increases the chances of successful treatment and better long-term outcomes. Here’s how doctors typically diagnose breast cancer:
-
Clinical Breast Examination
A healthcare provider checks the breasts and underarm areas for lumps, swelling, skin changes, or any unusual signs. This is usually the first step if symptoms are present.
-
Mammography
A mammogram is an X-ray of the breast and is the most common screening tool for early detection.
It helps identify tumors that may be too small to feel. If something suspicious is seen, additional imaging may be recommended.
-
Breast Ultrasound
Ultrasound uses sound waves to create images of the breast.
It helps distinguish between:
- Solid lumps (which may be cancerous)
- Fluid-filled cysts (usually non-cancerous)
Ultrasound is especially helpful for women with dense breast tissue.
-
Breast MRI (Magnetic Resonance Imaging)
MRI offers highly detailed images and is used for:
- High-risk patients
- Evaluating the extent of cancer
- Clarifying unclear results from other imaging tests
It is often used along with mammography rather than as a standalone test.
-
Biopsy (The Confirmatory Test)
A biopsy is the only way to definitively diagnose breast cancer.
A doctor removes a small sample of breast tissue and sends it to a laboratory to check for cancer cells. Types of biopsy include:
- Fine-needle aspiration
- Core needle biopsy
- Surgical biopsy
The lab also determines the type, grade, and hormone receptor status of the cancer.
-
Additional Tests After Diagnosis
If cancer is confirmed, further tests help determine the stage and spread, such as:
- CT scans
- PET scans
- Bone scans
- Blood tests
How Is Breast Cancer Treated?
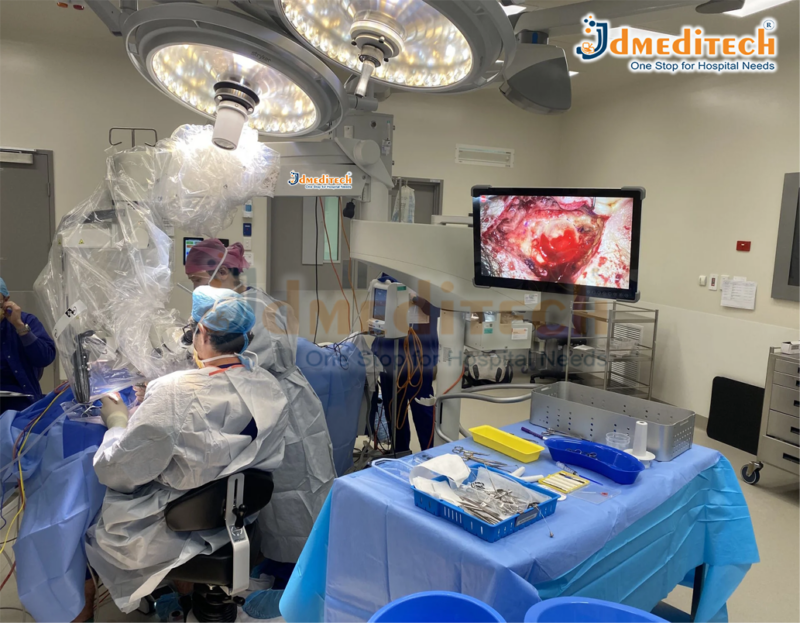
Breast cancer treatment depends on the type, stage, and size of the tumor and whether it has spread to other parts of the body. Doctors also consider the patient’s overall health and personal preferences. Most treatment plans involve a combination of therapies to remove the cancer, stop its growth, and reduce the chance of it returning.
-
Surgery
Surgery is often the first step in treating breast cancer. Common options include:
- Lumpectomy: Removes only the tumor and a small margin of surrounding tissue.
- Mastectomy: Removes the entire breast when the cancer is large or widespread.
- Lymph Node Removal: Checks if cancer has spread to lymph nodes.
Some patients may choose breast reconstruction surgery after a mastectomy.
-
Radiation Therapy
Radiation uses high-energy beams to destroy remaining cancer cells after surgery.
It helps reduce the risk of the cancer coming back in the same area.
-
Chemotherapy
Chemotherapy involves anti-cancer drugs given orally or through an IV.
It is used to:
- Shrink tumors before surgery
- Kill remaining cancer cells after surgery
- Treat cancers that have spread
Chemotherapy is especially important for aggressive types like triple-negative breast cancer.
-
Hormone (Endocrine) Therapy
Many breast cancers grow in response to hormones like estrogen or progesterone.
Hormone therapy blocks these hormones or lowers their levels.
It is effective for hormone receptor-positive cancers.
-
Targeted Therapy
Targeted drugs focus on specific proteins or genes that help cancer grow.
For example, HER2-positive breast cancer is treated with medicines that block the HER2 protein.
These treatments usually cause fewer side effects than chemotherapy.
-
Immunotherapy
Immunotherapy helps the body’s immune system recognize and attack cancer cells.
It is used for certain types of advanced or triple-negative breast cancer.
-
Supportive & Palliative Care
Supportive treatments help manage symptoms, improve comfort, and maintain quality of life.
This may include pain management, counseling, nutrition support, and physical therapy.
Conclusion
Breast cancer is a serious but treatable condition when identified early. Awareness, routine screenings, and healthy lifestyle choices play a crucial role in prevention and early diagnosis. If you or someone you know is at risk, consult a healthcare provider for guidance on screenings and preventive measures.
Explore More Product >>
Get Connected:
+91 79909 93062 | +91 63513 72032 | exports@jdmeditech.com