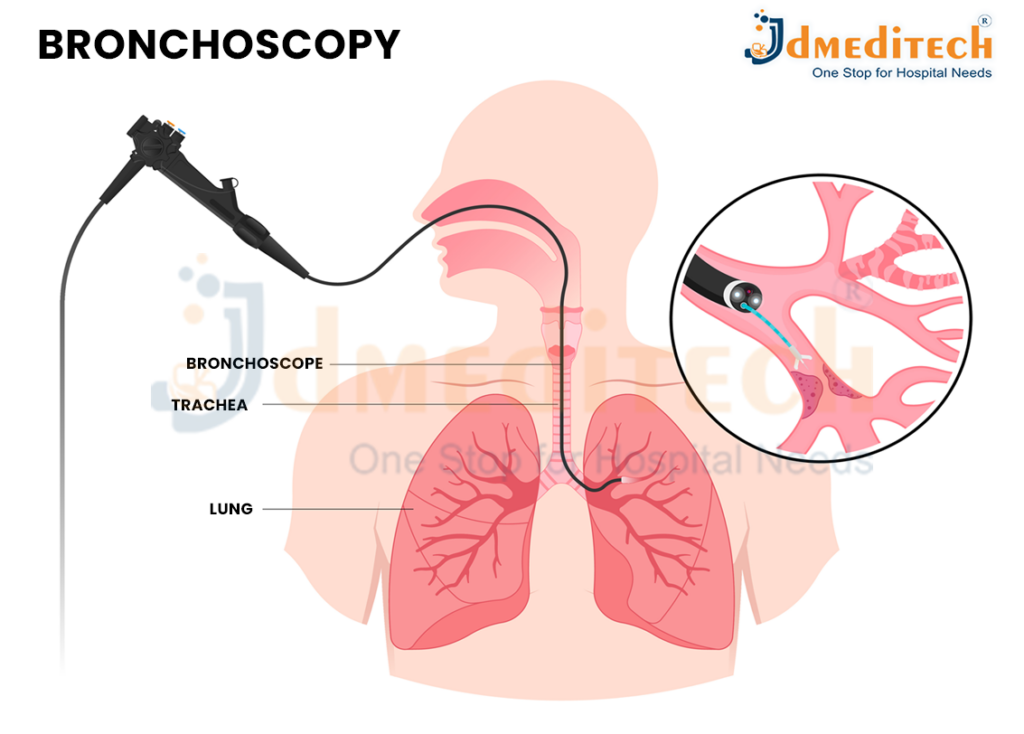
A bronchoscopy is a medical procedure using a thin, lighted tube (bronchoscope) inserted via the nose or mouth to view, diagnose, and treat lung and airway problems like infections, tumors, and blockages or to take tissue samples (biopsy). Done with sedation, it allows doctors to see inside the lungs, take samples, clear mucus, or even place stents, often on an outpatient basis. Patients usually go home the same day but need someone to drive them due to sedation.
What Is Bronchoscopy?
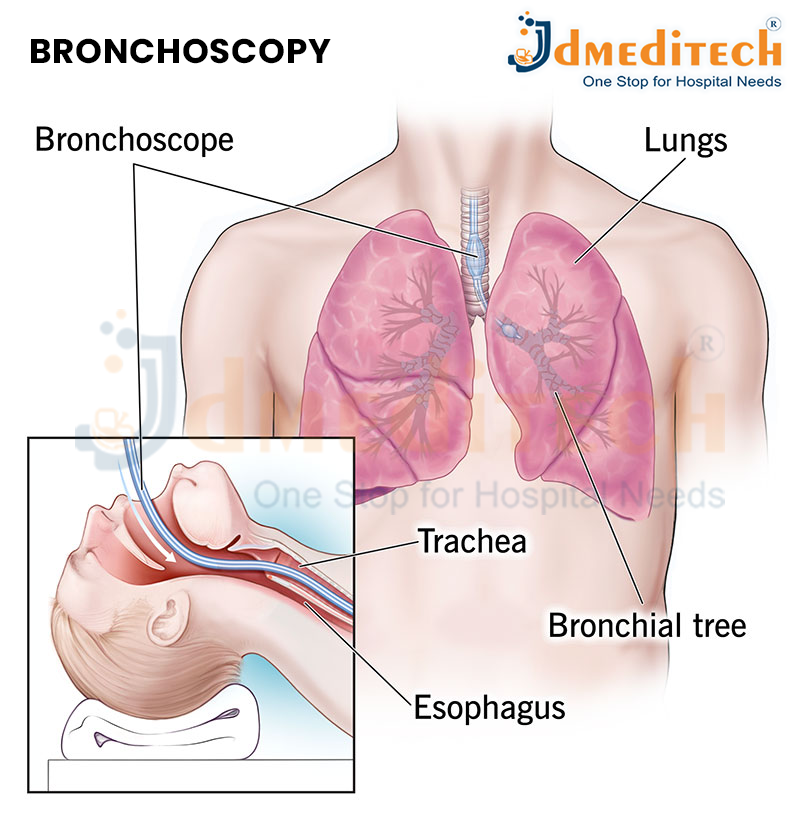
Bronchoscopy is an endoscopic examination in which a bronchoscope is inserted through the nose or mouth, down the throat, and into the lungs. The device has a tiny camera and light that help doctors visualize the airway lining.
It can be performed using:
- Flexible bronchoscopy: Most common; used for diagnosis and minor treatments.
- Rigid bronchoscopy: Used for more complex situations, such as removing large obstructions or controlling heavy bleeding.
How Is Bronchoscopy Performed?
-
Preparation
The patient is asked to avoid food and drink for a few hours before the procedure. A local anesthetic is sprayed into the throat, and mild sedation is given.
-
Procedure
- The bronchoscope is gently inserted through the nose or mouth.
- The doctor examines the windpipe and bronchi while watching the video monitor.
- If required, samples of mucus or tissue are collected.
-
Duration
The procedure typically lasts 20–45 minutes, depending on the purpose.
What Happens During a Bronchoscopy?
During a bronchoscopy, a doctor examines your airways and lungs using a thin tube called a bronchoscope. The procedure is usually done in a hospital or clinic and takes about 20–45 minutes. Here’s what typically happens step-by-step:
-
Preparation Before the Procedure
- You will be asked not to eat or drink for a few hours before the bronchoscopy.
- A local anesthetic is sprayed in your nose and throat to numb the area.
- You may receive a mild sedative through an IV to help you relax.
-
Inserting the Bronchoscope
- The doctor gently inserts the bronchoscope through your nose or mouth.
- It then moves down your throat, into the windpipe (trachea), and finally into the bronchi (airways of the lungs).
-
Visual Examination
- The bronchoscope has a tiny camera and light.
- The doctor views the airways on a video screen, checking for:
- Inflammation
- Infection
- Bleeding
- Tumors or abnormal growths
- Blockages
-
Collecting Samples (If Needed)
The doctor may take:
- Biopsy (small tissue samples)
- Mucus or fluid samples (bronchoalveolar lavage)
- Brushings from the airway walls
These samples help diagnose infections, cancer, inflammation, or other lung diseases.
-
Treatment During Bronchoscopy (If Required)
In some cases, bronchoscopy is used to perform treatments such as:
- Removing mucus plugs or foreign objects
- Controlling bleeding
- Opening narrow airways
- Delivering medication directly into the lungs
-
Completion of the Procedure
- The bronchoscope is carefully removed.
- You will be taken to a recovery area until the sedative wears off.
- Throat numbness or mild coughing is normal for a few hours.
Conclusion
Bronchoscopy is a valuable diagnostic and therapeutic procedure that provides a clear view of the lungs and airways. It helps doctors diagnose complex respiratory issues and guide treatment effectively. If you have persistent breathing problems, coughing, or unexplained chest abnormalities, your doctor may recommend this safe and reliable procedure.