Cataract Surgery
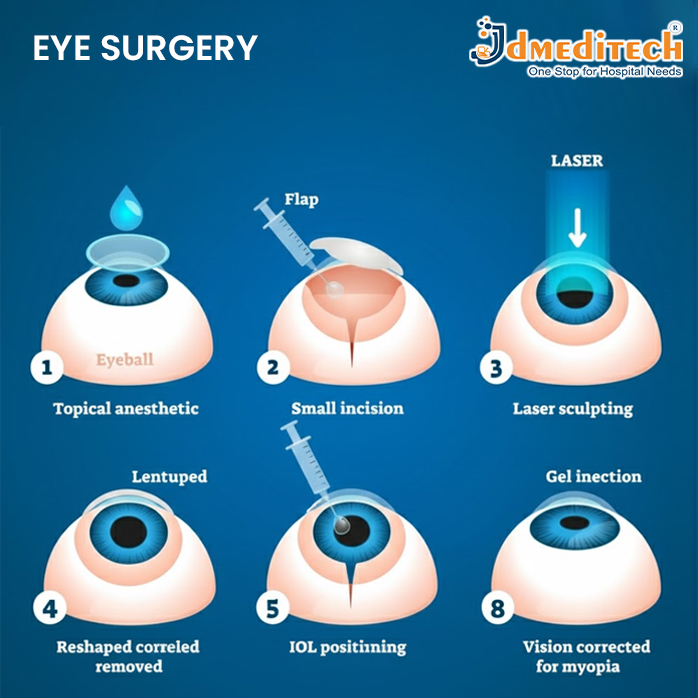
Cataract surgery is a safe and commonly performed eye procedure used to remove a cloudy natural lens from the eye and replace it with a clear artificial lens called an Intraocular Lens (IOL). A cataract forms when the eye’s lens becomes cloudy due to aging, injury, or medical conditions like diabetes. This cloudiness causes blurred vision, glare, faded colors, and difficulty seeing at night.
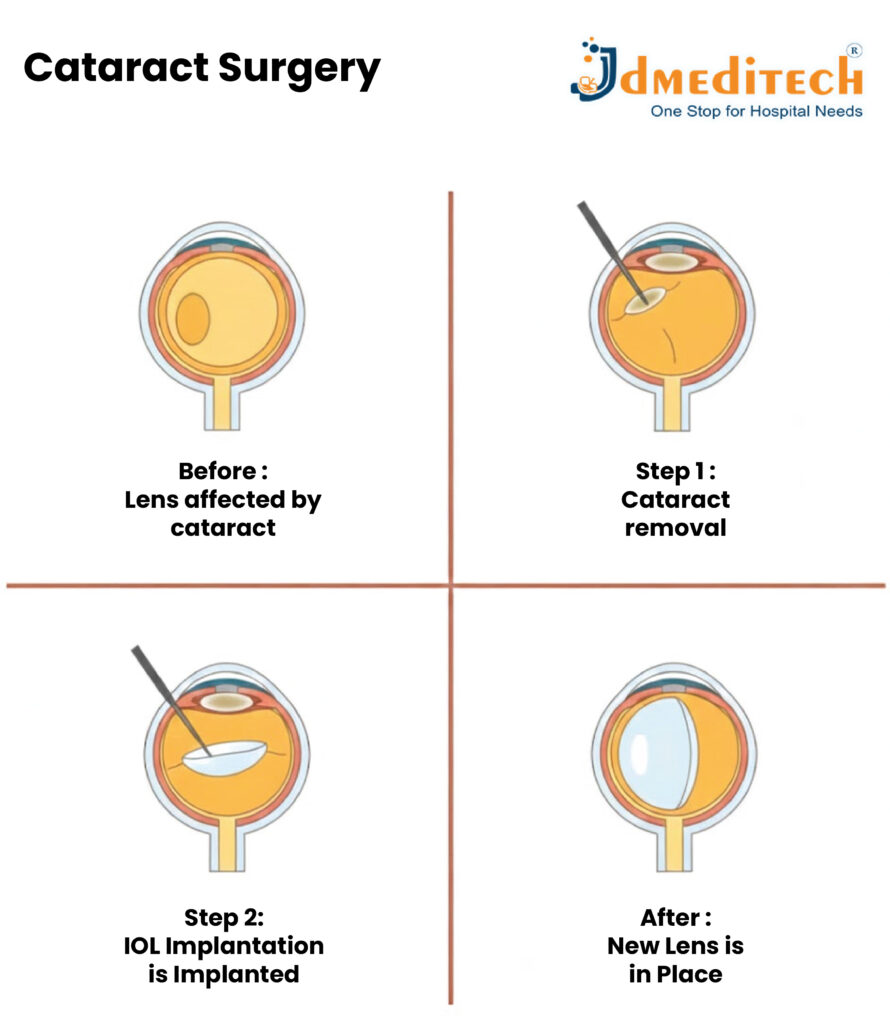
During cataract surgery, the doctor makes a very small incision on the eye and gently breaks the cloudy lens using a technique called phacoemulsification. The clouded lens is then removed, and a new artificial lens is inserted in the same place to restore clear vision. The procedure is usually painless, performed under local anesthesia, and takes about 15–20 minutes.
What to Expect Before & After Surgery
- You may be asked to stop eating or drinking for a certain period before surgery, and some medications (especially blood thinners) may need to be paused temporarily.
- The procedure usually takes a short time and is done under local anesthesia, so it’s generally painless.
- After surgery, vision may be blurry for a few days while the eye heals. Colors may appear brighter once the eye adjusts.
- You’ll be given eye drops (for infection prevention / inflammation control) and likely asked to avoid rubbing the eye, heavy lifting, or strenuous activity for a short period.
When Should You Have Cataract Surgery?
You should consider cataract surgery when cataracts start affecting your daily life or causing significant vision problems. Here are the main situations:
-
Difficulty in daily activities
- Blurry or cloudy vision
- Trouble reading
- Difficulty watching TV or using your phone
- Problems doing regular tasks
-
Trouble driving at night
- Increased glare from headlights
- Poor night vision
- Difficulty seeing road signs clearly
-
Colors appear faded or dull
Cataracts make the lens cloudy, so colors no longer look bright or clear.
-
Glasses no longer improve your vision
If changing your eyeglass prescription does NOT improve clarity, surgery becomes necessary.
-
A cataract becomes “mature.”
When the lens becomes too cloudy (mature cataract), delaying surgery can make it more difficult later.
-
If you have other eye diseases
People with diabetes, glaucoma, or retinal issues should get timely treatment to protect their vision.
Is Cataract Surgery Right for You?
Cataract surgery is generally recommended when the cataract interferes significantly with daily life—for example, when you struggle to read, drive, recognize faces, or perform tasks due to poor vision.
It’s a decision best made in consultation with an experienced ophthalmologist, after a full eye examination and understanding of your overall health.
Because the procedure is highly effective—with a success rate of over 90% (many studies quote ~95–98%)—the benefits often outweigh the risks for most people.
Conclusion
Cataract surgery is a remarkable medical advancement—a safe, routine procedure that can restore sight, brighten colors, reduce glare, and improve independence and quality of life. While there are some risks, complications are rare, and most patients enjoy excellent results with proper care.
If you or a loved one notice gradually worsening vision, trouble with glare, dull colors, or difficulty with daily tasks—it might be time to consult an eye specialist. And with trusted equipment providers like your company, good quality surgical instruments and lenses play a vital role in delivering safe, effective care.